Pelvic Health 101: Why It Matters and What Every Woman Should Know
When we talk about women's health, conversations often centre around hormones, fertility or digestion - one area that’s quietly connected to them all is often overlooked: the pelvic floor.
Pelvic health isn’t just about childbirth or bladder leaks. It’s about understanding the deep connection between your core, your breath, your digestion, and your sense of strength and confidence in your own body.
If you’ve ever struggled with bloating, discomfort, or core weakness or simply want to feel more aligned and connected this guide will help you understand what pelvic health is, why it matters, and how to start supporting it.
What Is Pelvic Health?
Your pelvic floor is a group of muscles, ligaments, and connective tissues that sit at the base of your pelvis, forming a kind of supportive “hammock” for your bladder, uterus, and bowels.
When these muscles work as they should, they:
Support your internal organs
Help control bladder and bowel function
Stabilize your spine and hips
Enhance sexual function
Support posture and movement
But when the pelvic floor is weak, tight, or uncoordinated, it can lead to issues like back pain, constipation, urinary urgency, or even discomfort during sex.
Why Pelvic Health Deserves More Attention
For many women, the pelvic floor only becomes a topic of conversation after giving birth or noticing symptoms. But the truth is, pelvic health impacts every stage of life from your first period to menopause and beyond.
This system is deeply connected to your core muscles, diaphragm, and digestion. When one is out of balance, the others often are too.
A few ways your pelvic floor may influence your overall health:
Digestive health: Chronic bloating, constipation, or straining can all affect or be affected by pelvic muscle tone.
Hormonal health: Shifts in estrogen (especially around the menstrual cycle or menopause) may change tissue strength, as there are estrogen receptors on the pelvic floor muscles. Still, estrogen isn’t an independent risk factor. Our bodies are more complex. Factors like muscle strength, childbirth history, connective tissue health and more all likely contribute.
Stress and tension: Just like your shoulders or jaw, the pelvic floor can hold emotional and physical stress.
The Connection Between Pelvic Health, PCOS, and Gut Health
If you have PCOS or a sensitive gut, you might notice more bloating, inflammation, or pelvic discomfort, and that’s not your imagination.
Research shows that the hormonal and metabolic changes that come with PCOS (like higher insulin levels or inflammation) can affect how the pelvic floor muscles work. These muscles support your bladder, uterus, and bowel, so when they’re tense or not working properly, you might experience:
Pelvic tightness or cramping
Constipation or slower digestion
A feeling of heaviness or pressure in your lower abdomen
A 2023 review found that women with PCOS may be more likely to experience pelvic floor dysfunction (things like leakage with coughing or pelvic organ prolapse), although some hormone patterns like hyperandrogenism in PCOS may actually offer some protection!
Taking care of your pelvic floor health through gentle movement, stretching, breathwork, and working with a pelvic floor physiotherapist can help improve circulation, reduce inflammation, and support better gut and hormone health over time.
How to Support Your Pelvic Health Naturally
You don’t have to wait until symptoms show up to start caring for this area. Here are a few ways to begin reconnecting with your pelvic floor:
1. Breathe Deeply
Your diaphragm and pelvic floor move together with every breath. Try placing a hand on your belly and one on your ribs. As you inhale, feel the belly and ribs expand; as you exhale, allow your body to soften. This mindful breathing helps retrain coordination between your breath and core.
2. Check Your Posture
Your pelvic floor thrives on alignment. When your posture is slouched or tilted, certain muscles overwork while others weaken. Gentle core strengthening and mobility work can help restore balance.
3. Stay Hydrated and Regular
Constipation is one of the most common contributors to pelvic tension. Prioritize hydration, fibre-rich foods, and regular meals to support better functioning digestion.
4. Move Mindfully
Low-impact exercise like yoga, Pilates, or walking can enhance circulation and reduce tension. If you experience discomfort, pelvic health physiotherapy can guide you through safe, restorative movements tailored to your body.
5. Listen to Your Body
If you feel heaviness, pain, or pressure in your pelvis or if you’re frequently “holding in” stress your body may be asking for support. Remember: awareness is the first step toward healing.
When to See a Pelvic Health Physiotherapist
A pelvic health physiotherapist specializes in assessing how your pelvic floor muscles function and helping you regain strength, mobility, and confidence.
You might benefit from seeing one if you experience:
Urinary leakage or urgency
Constipation or straining
Pain during sex
Pelvic pressure or heaviness
Postpartum discomfort or diastasis recti
An appointment often includes gentle education, breathing techniques, and personalized exercises no shame, no rush, just understanding and support.
We have a trusted network of pelvic floor physiotherapists, please reach out for a referral!
The Bottom Line
Your pelvic floor is part of your body’s foundation; it supports your core, your hormones, and your overall well-being. By learning about it, you’re not just preventing future issues, you're strengthening your connection to your body.
Taking care of your pelvic health is important. Small, consistent habits can lead to greater comfort, confidence, and balance inside and out.
Ready to Learn More?
If you’re curious about how pelvic health connects to digestion, hormones, and energy, keep an eye out for upcoming resources and expert insights including tips from leading pelvic health physiotherapists and women’s wellness practitioners.
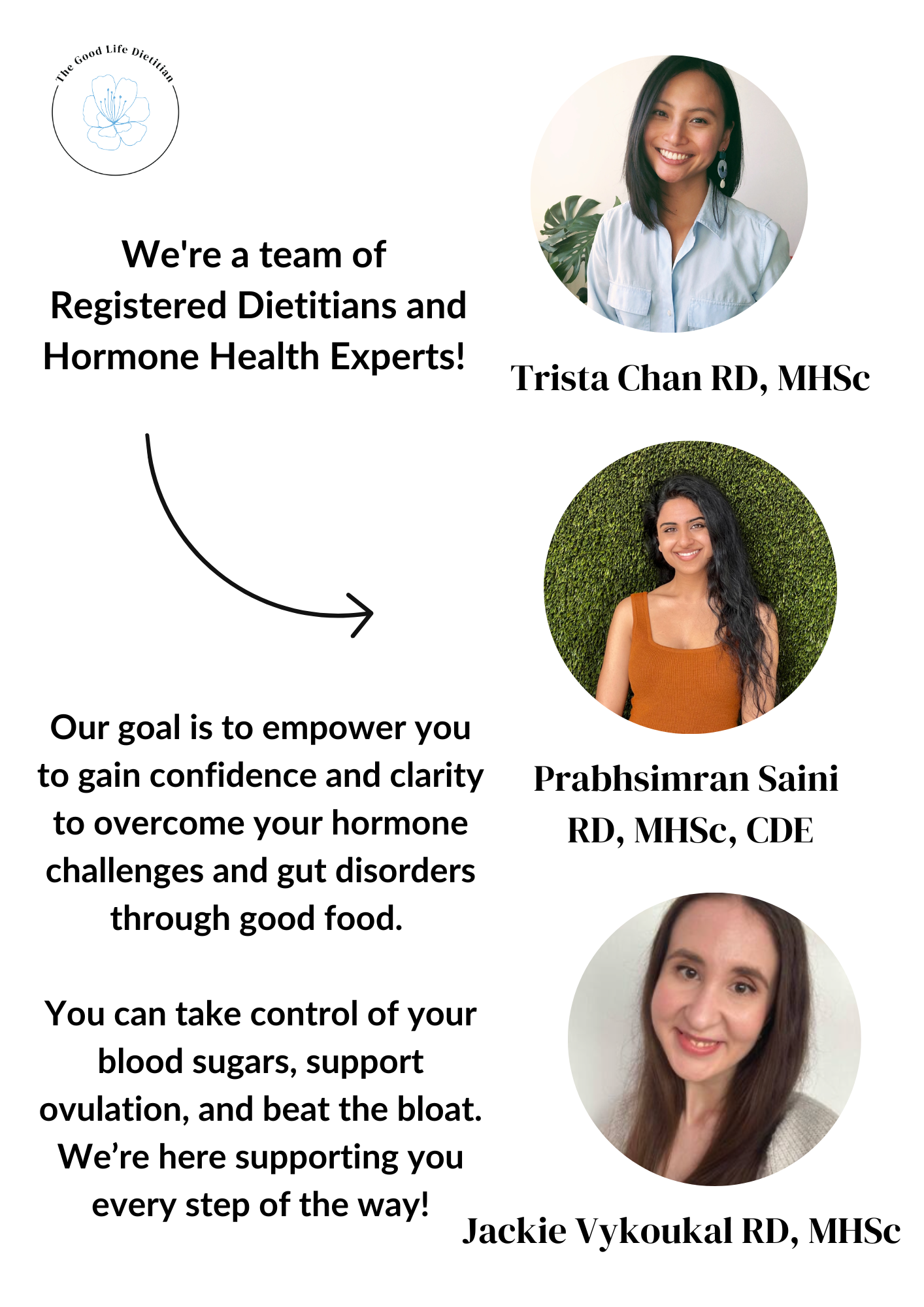
Hi! I’m Trista
A Registered Dietitian and reproductive health expert. I’m here to help you gain confidence to overcome your Polycystic Ovary Syndrome and digestive health woes, while bettering your relationship with food.
CATEGORIES
Ready for Support?
If you’re craving a calmer, more sustainable approach to nutrition, our dietitians’ 1-on-1 nutrition programs can help you personalize gentle nutrition, stabilize energy and digestion, and build habits that last - no rigid rules required.
References
Dietz, H.P., Socha, M., Atan, I.K. et al. Does estrogen deprivation affect pelvic floor muscle contractility?. Int Urogynecol J 31, 191–196 (2020). https://doi.org/10.1007/s00192-019-03909-w
Saei Ghare Naz M, Ramezani Tehrani F, Behroozi-Lak T, Mohammadzadeh F, Kholosi Badr F, Ozgoli G. Polycystic Ovary Syndrome and Pelvic Floor Dysfunction: A Narrative Review. Res Rep Urol. 2020;12:179-185